Case of a Left Ventricular Free Wall Rupture - Occurred as a late complication of lateral ST-elevation myocardial infarction
We came across an interesting case of left ventricular free wall rupture at our institution. The occurrence of left ventricular free wall rupture in acute myocardial infarction decreased with the extent of interventional procedures of reperfusion, but it is still encountered in 1-2% of these patients. We are presenting the case of 55 years old male with left ventricular free wall rupture occurred as a late complication of lateral ST-elevated myocardial infarction. The aim of this case report is to highlight the main clinical features, the diagnostic value of the echocardiographic exam and the importance of early surgical intervention in a rare, but very dangerous condition, with persistent high mortality rates. In this context, we will review the current prevalence, clinical forms and prediction factors of left ventricular free wall rupture.
The coronary angiogram was done which showed occluded diagonal and rest of the vessels had no significant angiographic disease. The patient was transferred in the department of cardiovascular surgery for the intervention of LVFWR repair. The pericardium was opened via a median sternotomy. A significant amount of clot and blood was removed. The lateral wall left ventricular fissured pseudoaneurysm was confirmed and carefully dissected only after the heart was discharged on cardiopulmonary bypass. The slit like rupture was sealed by thrombus and it should be considered that this feature is the main reason for the avoidance of a sudden rupture and death. A composite Dacron with autologous pericardium patch was used for LVFWR repair. The geometry of the left ventricle was restored. In postoperative period he required inotropic support and IABP which were gradually weaned off and the patient was discharged after seven days of hospitalization.
The patient started to keep appropriate diet, and followed a pharmacological treatment with a beta-blocker, aspirin, an ACE-inhibitor and a statin.
There is consistent data indicating that primary PCI in acute myocardial infarction is the most important protective factor against a cardiac rupture (1, 2, 4, and 7). In series of 5699 patients with acute myocardial infarction Honda et al. have analyzed the clinical and pathological trends of cardiac rupture on three cohorts characteristic for the following periods of time: 1977-1989, 1990-2001 and 2001-2011. The incidence of this complication decreased concomitantly with the widespread application of reperfusion therapy, from 3.3% in the first cohort to 1.7% in the last one (2). Recently, similar conclusions have been revealed by Chang RY et al. In their study, conducted between 1999 and 2013, they have reported that LVFWR was significantly lower in patients with ST-elevated myocardial infarction submitted to primary PCI than in patients who have received thrombolysis or pharmacologic treatment alone (7).
Regarding risk factors there is a large agreement that advanced age (>70 years old) or female sex are predictors of risk for LVFWR (2-4, 6). Other factors have been associated with the risk of LVFWR in different studies: first myocardial infarction (2, 18), Killip class > 2 at presentation (4, 6-7), initial high levels of myocardial biomarkers (3, 6) or poor coronary collateralization (18).
In our case we should consider that the lack of early revascularization, due to a neglected acute coronary syndrome, was the main contributing factor to LVFWR.
In the presented case the localization of LVFWR was on the lateral wall. Data from early studies have indicated anterior wall as the most common topography of LVFWR (2). In the last years some authors have emphasized the involvement of the lateral wall segment as well, that can reach 28% of cases for the lateral wall (5). In our patient LVFWR has occurred in the context of one-vessel coronary artery disease i.e. occluded diagonal.
The pathologic substrate of LVFWR consists in intramyocardial hemorrhage and microvascular obstruction (11). Beyond ischemia, the occurrence of these lesions can be influenced by two other factors: the quality of the collateral circulation (17, 20) and the balance between extracellular matrix and the expression of metalloproteinases (MMPs) (15). Accordingly, the sex influence on myocardial rupture could be explained by less developed collaterals in women than in men (21), while the age risk could derive from an inflammatory status prone to the activation of MMPs (15). It is considered that all these conditions are contributing to the decrease in tensile strength of the infarcted myocardium.
In the presented case the diagnosis of myocardial rupture was realized promptly based on echocardiographic examination, for which was reported a 100% sensitivity and a 93% specificity for the detection of this complication (22). In a study conducted by Figueras et al. the mean SD of pericardial width of 22.2 mm has been associated with a higher probability of hemodynamic instability versus 16.3 mm (23).
LVFWR is still associated with high mortality rates (50-60%) (2, 6) accounting for 95% of electromechanical dissociation in patients with acute myocardial infarction (24). Prompt surgical intervention can be life-saving, ensuring survival for a long period of time, as it was emphasized in our report.
1. Moreno R, López-Sendón J, García E, et al. - Primary angioplasty reduces the risk of left ventricular free wall rupture compared with thrombolysis in patients with acute myocardial infarction. J Am Coll Cardiol. 2002;39:598–603. [PubMed]
2. Honda S, Asaumi Y, Yamane T, et al. - Trends in the clinical and pathological characteristics of cardiac rupture in pati ents with acute myocardial infarction over 35 Years. J Am Heart Assoc. 2014;3:e0984. [PMC free article] [PubMed]
3. López-Sendón J, Gurfi nkel EP, López de Sá E, et al. - Factors related to heart rupture in acute coronary syndromes in Global Registry of Acute Coronary Events. Eur Heart J. 2010;31:1449–1456. [PubMed]
4. Gueret P, Khalife K, Jobic Y, et al. - Echocardiographic assessment of the incidence of mechanical complications during the early phase of myocardial infarction in the reperfusion era: a French multicentre prospective registry. Arch Cardiovasc Dis. 2008;101:41–7. [PubMed]
5. Exadaktylos NI, Kranidis AI, Argyriou MO, et al. - Left ventricular free wall rupture during acute myocardial infarction. Early diagnosis and treatment. Hellenic J Cardiol. 2002;43:246–52.
6. French JK, Hellkamp AS, Armstrong PW, et al. - Mechanical complications after percutaneous coronary intervention in ST-elevation myocardial infraction (from APEX-AMI). Am J Cardiol. 2010;105:59–63. [PubMed]
7. Chang RY, Tsai HL, Hsiao PG, et al. - Comparison of the risk of left ventricular free wall rupture in Taiwanese patients with ST-elevation acute myocardial infarction undergoing diff erent reperfusion strategies: A medical record review study. Medicine (Baltimore). 2016;95:e5308. [PMC free article] [PubMed]
8. Hosseinzadeh-Maleki M, Valizadeh N, Rafatpanah N, Moezi SA. - Survival after left ventricular free wall rupture due to acute myocardial infarction. ARYA Atheroscler. 2015;11:310–3. [PMC free article] [PubMed]
9. Fent G, Grech E, Parviz Y, Briff a N. - Left ventricular free wall rupture complicating acute STEMI. Acute Cardiac Care. 2015;17:45. [PubMed]
10. Che Y, Li G, Chen K, Liu T. - Post-MI free wall rupture syndrome. Case report, literature review, and new terminology. Clin Case Rep. 2016;4:576–83. [PMC free article] [PubMed]
11. Garg P, Saif-El-Dean AR, Greenwood JP, Plein S. - Free-Wall Rupture Post-Reperfused Acute Myocardial Infarction: Insights from Multimodality Cardiovascular imaging. Circulation. 2015;132:e245–7. [PubMed]
12. Duke M. - An historical review of rupture of heart. Conn Med. 1993;57:91–96. [PubMed]
13. Purcaro A, Costantini C, Ciampani N, et al. - Diagnostic criteria and management of subacute ventricular free wall rupture complicating acute myocardial infarction. Am J Cardiol. 1997;80:397–405. [PubMed]
14. Becker AE, van Mantgem JP. - Cardiac tamponade. A study of 50 hearts. Eur J Cardiol. 1975;3:349–58. [PubMed]
15. Raynolds HR, Hochman JS. - Heartbreak. Eur Heart J. 2010;31:1433–35. [PubMed]
16. Hutchins KD, Skurnick J, Lavenhar M, Natarajan GA. - Cardiac rupture in acute cardiac infarction: a reassessment. Am J Forensic Med Pathol. 2002;23:78–82. [PubMed]
17. Frances C, Romero A, Grandi D. - Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998;32:357–61.
18. Yip HK, Wu CJ, Chang HW, et al. - Cardiac rupture complicating direct percutaneous reperfusion coronary intervention in reperfusion era. Chest. 2003;124:565–571. [PubMed]
19. Reardon MJ, Carr CL, Diamond A, et al. - Ischemic left ventricular free wall rupture: prediction, diagnosis and treatment. Ann Thorac Surg. 1997;64:1509–1513. [PubMed]
20. Pretre R, Rickli H, Ye Q, et al. - Frequency of collateral blood fl ow in the infarctrelated coronary artery in rupture of the ventricular septum after acute myocardial infarction. Am J Cardiol. 2000;85:497–499. [PubMed]
21. Johansson S, Bergstrand R, Schlossman D et al. - Sex diff erences in cardioangiographic fi ndings after myocardial infarction. Eur Heart J. 1984;5:374–381. [PubMed]
22. López-Sendón J, Gonzáles A, López de Sá E, et al. - Diagnosis of subacute ventricular wall rupture after acute myocardial infarction: sensitivity and specifi city of clinical, hemodynamic and echocardiographic criteria. J Am Coll Cardiol. 1992;19:1145–53. [PubMed]
23. Figueras J, Cortadellas J, Soler-Soler J, et al. - Left ventricular free wall rupture: clinical presentation and management. Heart. 2000;83:499–504. [PMC free article] [PubMed]
24. Figueras J, Curos A, Cortadellas J, Soler-Soler J. - Reliability of electromechanical dissociation in the diagnosis of left ventricular free wall rupture in acute myocardial infarction. Am Heart J. 1996;131:861–64. [PubMed]
Introduction:
It has been reported that with the extension of interventional procedures of reperfusion the occurrence of left ventricular free wall rupture (LVFWR) is decreased (1, 2). However, it is still encountered in less than 2% of cases with ST-elevated acute myocardial infarction (3-7), even after urgent reperfusion therapy (8-11), and is associated with high mortality rates (3,6). With this case report we aim to remind the importance of early recognition and surgical intervention in this life-threatening condition.Case:
A 55 year old male was admitted to the hospital with intense chest pain, diaphoresis and hypotension, fifteen days after a resuscitated cardiac arrest at local hospital in his village after which he did not get medical attention. He had no history of smoking, diabetes mellitus or hypertension. ECG showed Q waves in lead I, aVL with 1 mm ST-segment elevation and ST segment depressions in V4, V5 and V6 leads indicating previous lateral wall myocardial infarction. High levels of Troponin I and a normal level of CK-MB have been recorded in the emergency unit. Echocardiographic study was immediately performed, showing a lateral wall rupture with pseudo-aneurysm of the lateral wall, hemopericardium and intrapericardial thrombus sealing lateral wall rupture (Figure 1 and Figure 2). The maximum width of the pericardial effusion was 20 mm.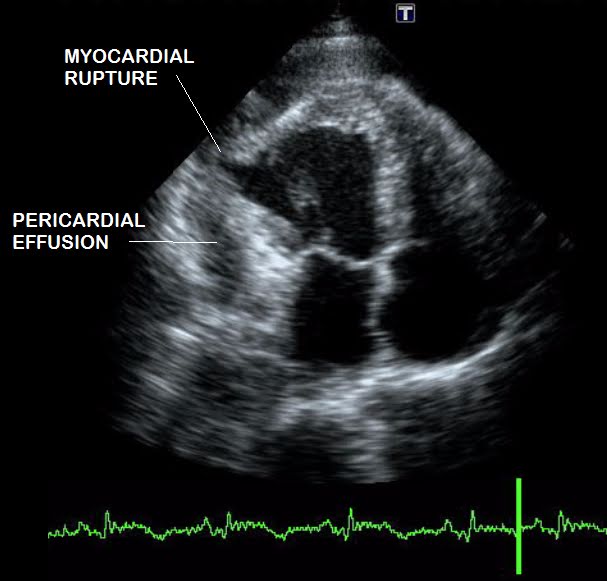 |
| Figure 1: Echocardiographic evaluation showing pseudoaneurysm and rupture of the lateral wall with hemopericardium and intrapericardial thrombus |
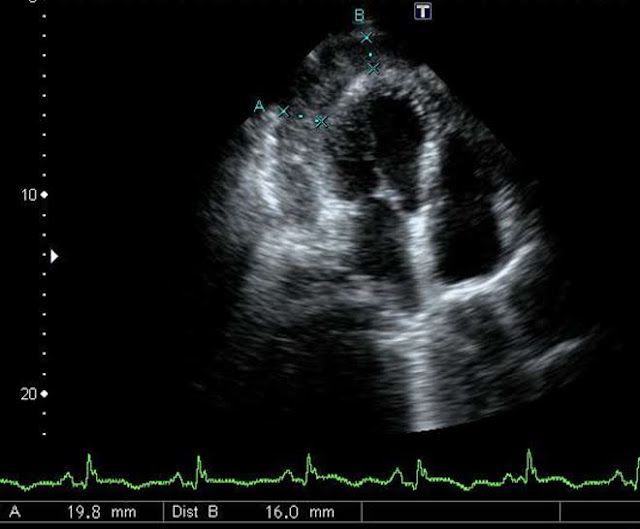 |
| Figure 2: Lateral wall rupture concealed by a thrombus |
 |
| Figure 3: Coronary Angiography showing occluded diagonal. |
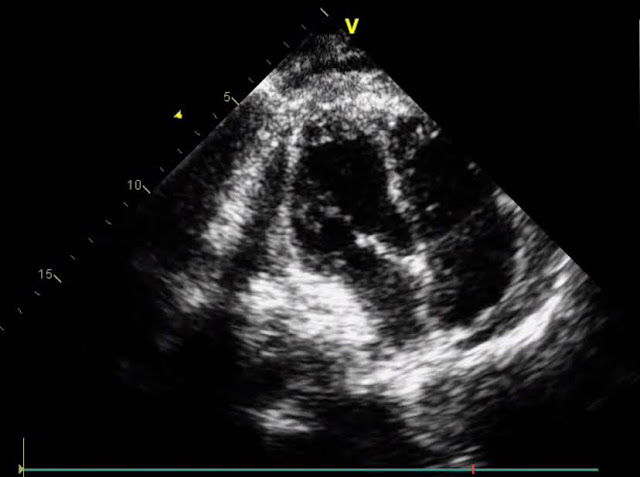 |
| Figure 4: Echocardiographic evaluation after surgical repair of the free wall |
The patient started to keep appropriate diet, and followed a pharmacological treatment with a beta-blocker, aspirin, an ACE-inhibitor and a statin.
Discussion:
Left ventricular free wall rupture (LVFWR) usually occurs between 24 hours to one week from the acute coronary event (13). In a randomized trial in which primary percutaneous coronary intervention (PCI) was the reperfusion therapy mechanical complications occurred at a median of 23.5 hours after the onset of symptoms (6). In the presented case we have considered the LVFWR as a late complication of a previous ignored myocardial necrosis due to lateral wall ST segment elevation MI which evolved into lateral pseudoaneurysm that finally cracked and generated hemopericardium with subsequent sealing of slit like opening with thrombus. This scenario is corresponding to type II free wall rupture in the classification of Becker and van Mantgem, the so-called “concealed rupture” which is suggestive of the slow tear of the myocardium and typically occurs more than 24 hours after the infarction. The infarcted myocardium erodes before rupture and is covered by a thrombus. The other two forms of LVFWR are the abrupt fissure (type I) - occurring usually early after infarction and the erosion in the area of a previously formed aneurysm (type II) (14, 15).There is consistent data indicating that primary PCI in acute myocardial infarction is the most important protective factor against a cardiac rupture (1, 2, 4, and 7). In series of 5699 patients with acute myocardial infarction Honda et al. have analyzed the clinical and pathological trends of cardiac rupture on three cohorts characteristic for the following periods of time: 1977-1989, 1990-2001 and 2001-2011. The incidence of this complication decreased concomitantly with the widespread application of reperfusion therapy, from 3.3% in the first cohort to 1.7% in the last one (2). Recently, similar conclusions have been revealed by Chang RY et al. In their study, conducted between 1999 and 2013, they have reported that LVFWR was significantly lower in patients with ST-elevated myocardial infarction submitted to primary PCI than in patients who have received thrombolysis or pharmacologic treatment alone (7).
Regarding risk factors there is a large agreement that advanced age (>70 years old) or female sex are predictors of risk for LVFWR (2-4, 6). Other factors have been associated with the risk of LVFWR in different studies: first myocardial infarction (2, 18), Killip class > 2 at presentation (4, 6-7), initial high levels of myocardial biomarkers (3, 6) or poor coronary collateralization (18).
In our case we should consider that the lack of early revascularization, due to a neglected acute coronary syndrome, was the main contributing factor to LVFWR.
In the presented case the localization of LVFWR was on the lateral wall. Data from early studies have indicated anterior wall as the most common topography of LVFWR (2). In the last years some authors have emphasized the involvement of the lateral wall segment as well, that can reach 28% of cases for the lateral wall (5). In our patient LVFWR has occurred in the context of one-vessel coronary artery disease i.e. occluded diagonal.
The pathologic substrate of LVFWR consists in intramyocardial hemorrhage and microvascular obstruction (11). Beyond ischemia, the occurrence of these lesions can be influenced by two other factors: the quality of the collateral circulation (17, 20) and the balance between extracellular matrix and the expression of metalloproteinases (MMPs) (15). Accordingly, the sex influence on myocardial rupture could be explained by less developed collaterals in women than in men (21), while the age risk could derive from an inflammatory status prone to the activation of MMPs (15). It is considered that all these conditions are contributing to the decrease in tensile strength of the infarcted myocardium.
In the presented case the diagnosis of myocardial rupture was realized promptly based on echocardiographic examination, for which was reported a 100% sensitivity and a 93% specificity for the detection of this complication (22). In a study conducted by Figueras et al. the mean SD of pericardial width of 22.2 mm has been associated with a higher probability of hemodynamic instability versus 16.3 mm (23).
LVFWR is still associated with high mortality rates (50-60%) (2, 6) accounting for 95% of electromechanical dissociation in patients with acute myocardial infarction (24). Prompt surgical intervention can be life-saving, ensuring survival for a long period of time, as it was emphasized in our report.
Conclusion:
The incidence of LVFWR has decreased with the widespread of reperfusion therapy in acute myocardial infarction. However, it can be still encountered, even after primary PCI, but more probably in patients who do not benefit from urgent interventional procedures of reperfusion. LVFWR occurs usually in the first 24 hours after acute myocardial infarction, in patients with advanced age, more frequently in females and on the anterior wall of the left ventricle, in the context of three-vessel coronary artery disease. We aimed to increase awareness for this life-threatening condition even in less expected situations, like that of the presented patient: male, younger than 70 years old, with one-vessel coronary artery disease and with the rupture localized in the lateral wall, evolving very late after the onset of the acute episode of myocardial ischemia and in the absence of primary reperfusion. The other two reasons for which we have reported this case were to remind the echocardiographic features of “concealed rupture” with fissured pseudoaneurysm, less illustrated in the last years than the acute forms of LVFWR (the abrupt fissure or the erosion) and to highlight the importance of prompt surgical intervention for the survival of patients with LVFWR.References:
1. Moreno R, López-Sendón J, García E, et al. - Primary angioplasty reduces the risk of left ventricular free wall rupture compared with thrombolysis in patients with acute myocardial infarction. J Am Coll Cardiol. 2002;39:598–603. [PubMed]
2. Honda S, Asaumi Y, Yamane T, et al. - Trends in the clinical and pathological characteristics of cardiac rupture in pati ents with acute myocardial infarction over 35 Years. J Am Heart Assoc. 2014;3:e0984. [PMC free article] [PubMed]
3. López-Sendón J, Gurfi nkel EP, López de Sá E, et al. - Factors related to heart rupture in acute coronary syndromes in Global Registry of Acute Coronary Events. Eur Heart J. 2010;31:1449–1456. [PubMed]
4. Gueret P, Khalife K, Jobic Y, et al. - Echocardiographic assessment of the incidence of mechanical complications during the early phase of myocardial infarction in the reperfusion era: a French multicentre prospective registry. Arch Cardiovasc Dis. 2008;101:41–7. [PubMed]
5. Exadaktylos NI, Kranidis AI, Argyriou MO, et al. - Left ventricular free wall rupture during acute myocardial infarction. Early diagnosis and treatment. Hellenic J Cardiol. 2002;43:246–52.
6. French JK, Hellkamp AS, Armstrong PW, et al. - Mechanical complications after percutaneous coronary intervention in ST-elevation myocardial infraction (from APEX-AMI). Am J Cardiol. 2010;105:59–63. [PubMed]
7. Chang RY, Tsai HL, Hsiao PG, et al. - Comparison of the risk of left ventricular free wall rupture in Taiwanese patients with ST-elevation acute myocardial infarction undergoing diff erent reperfusion strategies: A medical record review study. Medicine (Baltimore). 2016;95:e5308. [PMC free article] [PubMed]
8. Hosseinzadeh-Maleki M, Valizadeh N, Rafatpanah N, Moezi SA. - Survival after left ventricular free wall rupture due to acute myocardial infarction. ARYA Atheroscler. 2015;11:310–3. [PMC free article] [PubMed]
9. Fent G, Grech E, Parviz Y, Briff a N. - Left ventricular free wall rupture complicating acute STEMI. Acute Cardiac Care. 2015;17:45. [PubMed]
10. Che Y, Li G, Chen K, Liu T. - Post-MI free wall rupture syndrome. Case report, literature review, and new terminology. Clin Case Rep. 2016;4:576–83. [PMC free article] [PubMed]
11. Garg P, Saif-El-Dean AR, Greenwood JP, Plein S. - Free-Wall Rupture Post-Reperfused Acute Myocardial Infarction: Insights from Multimodality Cardiovascular imaging. Circulation. 2015;132:e245–7. [PubMed]
12. Duke M. - An historical review of rupture of heart. Conn Med. 1993;57:91–96. [PubMed]
13. Purcaro A, Costantini C, Ciampani N, et al. - Diagnostic criteria and management of subacute ventricular free wall rupture complicating acute myocardial infarction. Am J Cardiol. 1997;80:397–405. [PubMed]
14. Becker AE, van Mantgem JP. - Cardiac tamponade. A study of 50 hearts. Eur J Cardiol. 1975;3:349–58. [PubMed]
15. Raynolds HR, Hochman JS. - Heartbreak. Eur Heart J. 2010;31:1433–35. [PubMed]
16. Hutchins KD, Skurnick J, Lavenhar M, Natarajan GA. - Cardiac rupture in acute cardiac infarction: a reassessment. Am J Forensic Med Pathol. 2002;23:78–82. [PubMed]
17. Frances C, Romero A, Grandi D. - Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998;32:357–61.
18. Yip HK, Wu CJ, Chang HW, et al. - Cardiac rupture complicating direct percutaneous reperfusion coronary intervention in reperfusion era. Chest. 2003;124:565–571. [PubMed]
19. Reardon MJ, Carr CL, Diamond A, et al. - Ischemic left ventricular free wall rupture: prediction, diagnosis and treatment. Ann Thorac Surg. 1997;64:1509–1513. [PubMed]
20. Pretre R, Rickli H, Ye Q, et al. - Frequency of collateral blood fl ow in the infarctrelated coronary artery in rupture of the ventricular septum after acute myocardial infarction. Am J Cardiol. 2000;85:497–499. [PubMed]
21. Johansson S, Bergstrand R, Schlossman D et al. - Sex diff erences in cardioangiographic fi ndings after myocardial infarction. Eur Heart J. 1984;5:374–381. [PubMed]
22. López-Sendón J, Gonzáles A, López de Sá E, et al. - Diagnosis of subacute ventricular wall rupture after acute myocardial infarction: sensitivity and specifi city of clinical, hemodynamic and echocardiographic criteria. J Am Coll Cardiol. 1992;19:1145–53. [PubMed]
23. Figueras J, Cortadellas J, Soler-Soler J, et al. - Left ventricular free wall rupture: clinical presentation and management. Heart. 2000;83:499–504. [PMC free article] [PubMed]
24. Figueras J, Curos A, Cortadellas J, Soler-Soler J. - Reliability of electromechanical dissociation in the diagnosis of left ventricular free wall rupture in acute myocardial infarction. Am Heart J. 1996;131:861–64. [PubMed]

Comments
Post a Comment
Drop your thoughts here, we would love to hear from you